How I Caught It Early — My Real Talk on Staying Ahead with Western Medicine
I never thought I’d be the one to catch a serious health issue early—until I did. It wasn’t luck. It was regular check-ups, paying attention to small changes, and trusting science-backed Western medicine. Early detection saved me from worse outcomes. Now, I share what really helped: simple, practical steps that fit into real life. This isn’t a miracle story—just smart, proactive choices anyone can make. What I learned wasn’t from a dramatic emergency room visit or a sudden collapse. It came quietly, through a routine blood test and a doctor who listened. That moment changed how I view my health—not as something to fix when broken, but to protect before it breaks. This is the quiet power of early detection: not heroics, but consistency.
The Wake-Up Call: When Small Symptoms Meant Something Bigger
For months, I noticed little things—tiredness that didn’t go away with extra sleep, a slight ache in my side after meals, and unexplained weight loss. At first, I brushed them off. I was busy—managing a household, supporting my family, juggling daily responsibilities. Who isn’t tired? Who doesn’t have an occasional ache? I told myself it was stress, aging, or just the pace of life. But deep down, a small voice whispered that something wasn’t quite right. I wasn’t in pain, not exactly, but my body felt off in a way I couldn’t name. That feeling, vague as it was, became the first clue.
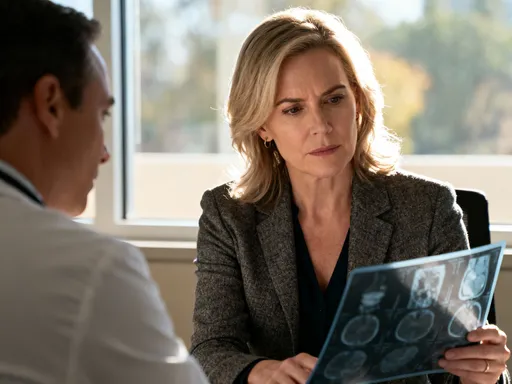
What changed was a routine annual check-up. My primary care physician, Dr. Patel, asked detailed questions—not just about symptoms, but about my energy levels, digestion, sleep quality, and family medical history. She didn’t dismiss my fatigue as normal. Instead, she ordered a full panel of blood tests and recommended an abdominal ultrasound. I admit, I hesitated. I felt fine, so why all the tests? But I trusted her approach. She explained that many conditions don’t announce themselves with dramatic symptoms. They start quietly, almost invisibly, and that’s exactly when they’re most treatable.
The results revealed elevated liver enzymes and a small, abnormal mass. Further imaging and a biopsy confirmed a rare but treatable condition that, if left undetected, could have led to serious complications. The diagnosis wasn’t cancer, but it was serious enough to require immediate attention. Because it was caught early, the treatment was minimally invasive and highly effective. Looking back, I realize how close I came to missing it. Those small symptoms weren’t just signs of a busy life—they were my body’s way of signaling that something needed medical evaluation. Western medicine’s diagnostic tools—lab work, imaging, and specialist consultations—made the difference between early intervention and advanced disease.
Why Early Detection Matters: What Science Actually Says
Medical research consistently shows that early detection improves outcomes across a wide range of conditions. According to the Centers for Disease Control and Prevention (CDC), detecting diseases in their initial stages often allows for simpler, less aggressive treatments and significantly increases survival rates. For example, when colorectal cancer is found at an early, localized stage, the five-year survival rate is about 90%. That number drops to 14% if the disease is not discovered until it has spread to distant organs. This isn’t an isolated case—similar patterns are seen with breast cancer, cervical cancer, and many chronic diseases.
Take type 2 diabetes. The American Diabetes Association emphasizes that many people live with undiagnosed diabetes for years because early symptoms can be mild or absent. During that time, high blood sugar silently damages blood vessels, nerves, and organs. But when caught early through routine screening—such as a fasting blood glucose test or HbA1c measurement—lifestyle changes and medication can prevent or delay complications like kidney disease, vision loss, and heart problems. Early intervention doesn’t just extend life; it preserves quality of life.
Hypertension, often called the “silent killer,” is another powerful example. It typically has no symptoms, yet it increases the risk of heart attack, stroke, and heart failure. The U.S. Preventive Services Task Force recommends regular blood pressure checks for all adults, especially those over 40 or with risk factors like family history or obesity. When high blood pressure is identified early, treatment with medication and lifestyle adjustments can normalize readings and reduce long-term risks. The science is clear: early detection is not about creating anxiety—it’s about gaining time, options, and control.
What makes Western medicine particularly effective in early detection is its reliance on evidence-based protocols. Screening guidelines are developed through large-scale studies and continuously updated based on new data. These aren’t arbitrary rules—they’re tools designed to catch problems before they become emergencies. By following them, individuals move from reactive to proactive health care, shifting the focus from crisis management to prevention.
My Go-To Screening Routine: What I Actually Do (And Why)
After my diagnosis, I committed to a consistent screening schedule. I didn’t wait for symptoms to return. Instead, I worked with my doctor to create a personalized plan based on my age, medical history, and risk factors. Here’s what I do now—and why each test matters.
Every year, I have a comprehensive physical exam. This includes measuring my blood pressure, checking my heart and lungs, and reviewing any new or ongoing symptoms. I also get a complete blood count (CBC) and a metabolic panel, which assess kidney and liver function, electrolyte balance, and blood sugar levels. These tests are simple—just a blood draw—but they provide a snapshot of my internal health. Abnormal results can signal infections, anemia, diabetes, or organ dysfunction long before symptoms appear.
Every two years, I undergo a lipid panel to monitor my cholesterol levels. High LDL cholesterol is a major risk factor for heart disease, the leading cause of death among women in the United States. My doctor uses these results to assess my cardiovascular risk and recommend dietary changes or medication if needed. I also have a thyroid function test every few years, as thyroid disorders are common in middle-aged women and can cause fatigue, weight changes, and mood swings.
For cancer screening, I follow established guidelines. I have a mammogram every year, as recommended for women over 40 by major health organizations. I also have a Pap smear and HPV test every five years to screen for cervical cancer. Colon cancer screening began at age 45 with a stool-based test, and I’ll transition to a colonoscopy in the coming years. These screenings aren’t optional in my mind—they’re essential maintenance, like changing the oil in a car. They don’t guarantee perfect health, but they dramatically increase the chances of catching problems early.
Depending on my results and family history, my doctor may recommend additional imaging, such as a bone density scan to check for osteoporosis or an ultrasound for liver or thyroid health. The key is consistency. These tests aren’t one-time events—they’re part of an ongoing relationship with my health care team. By staying on schedule, I avoid gaps in monitoring that could allow conditions to progress unnoticed.
Listening to Your Body Without Panicking: Spotting Red Flags Early
Being aware of your body doesn’t mean obsessing over every ache or sniffle. It means developing a baseline understanding of what’s normal for you so you can recognize when something is off. For years, I thought I had to be in pain to need medical attention. Now I know that subtle, persistent changes are often more telling than sudden, severe symptoms.
Some red flags are easy to overlook because they seem minor. Persistent fatigue that doesn’t improve with rest, unexplained weight loss or gain, changes in appetite or digestion, new or worsening headaches, and skin changes like rashes or unusual moles can all signal underlying conditions. So can changes in menstrual cycles, urinary habits, or sleep patterns. The key is not to jump to conclusions, but to document these changes and bring them to your doctor’s attention.
I keep a simple health journal where I note any unusual symptoms, their duration, and possible triggers. This helps me communicate clearly during appointments and avoids vague statements like “I just don’t feel right.” When I shared my journal with Dr. Patel, she was able to connect the dots between my fatigue, appetite changes, and lab results. Without that record, those clues might have been dismissed as stress or aging.
Western medicine encourages this kind of attentive self-monitoring—not as a substitute for professional evaluation, but as a complement to it. Your observations, combined with clinical testing, create a fuller picture of your health. The goal isn’t to diagnose yourself, but to be an informed partner in your care. By speaking up early, you give your doctor the information needed to act quickly and appropriately.
Building a Trusted Medical Team: Finding Doctors Who Listen
Not all doctors are the same. I’ve learned that the quality of care depends not just on medical expertise, but on communication, respect, and partnership. After my experience, I made it a priority to find providers who value prevention, take time to listen, and explain things clearly. This isn’t always easy, but it’s worth the effort.
When choosing a primary care physician, I looked for someone who asked open-ended questions, reviewed my full medical history, and encouraged me to speak up. I also wanted a doctor affiliated with a reputable medical system that offers coordinated care—access to specialists, labs, and imaging when needed. During my first visit, I asked about their approach to preventive care, screening schedules, and how they handle patient concerns. A doctor who welcomes questions is more likely to be a true partner in your health journey.
I also pay attention to how I’m treated during appointments. Do they make eye contact? Do they explain test results in plain language? Do they respect my time and concerns? If I feel rushed or dismissed, I don’t hesitate to seek a second opinion or change providers. Your doctor should be someone you trust, not someone you dread seeing.
Building a medical team also means knowing when to see specialists. After my diagnosis, I worked with a gastroenterologist who guided my treatment and follow-up care. I also consult a registered dietitian to support my nutritional health. These professionals work together, sharing records and insights, to provide comprehensive care. In Western medicine, coordination among providers is essential for managing complex or chronic conditions. By assembling a team that communicates well and values prevention, I’ve created a safety net that catches problems early.
Lifestyle Meets Medicine: How Daily Habits Support Early Warning Systems
Medical tests are powerful, but they work best when supported by a healthy lifestyle. I’ve learned that diet, sleep, physical activity, and stress management don’t replace medical care—they enhance it. When my body is in better balance, test results are more accurate, symptoms are easier to interpret, and my overall resilience improves.
I focus on a balanced diet rich in whole grains, lean proteins, fruits, and vegetables. I limit processed foods, added sugars, and excessive salt. This helps maintain stable blood pressure, cholesterol, and blood sugar levels—making it easier to spot true abnormalities in lab work. For example, if I eat poorly for weeks, my liver enzymes might rise temporarily, causing unnecessary concern. By eating well, I reduce false alarms and support long-term organ health.
Sleep is another cornerstone. I aim for seven to eight hours a night. Poor sleep can mimic or worsen symptoms like fatigue, brain fog, and mood changes—symptoms that might otherwise prompt a medical visit. By prioritizing rest, I give my body time to repair and regulate itself, making it easier to distinguish between lifestyle-related issues and genuine medical concerns.
Regular physical activity—walking, strength training, or yoga—keeps my heart strong, my weight stable, and my energy levels up. Exercise also reduces inflammation, a factor in many chronic diseases. When I stay active, my doctor can more accurately assess whether a symptom is due to deconditioning or something more serious. At the same time, I manage stress through mindfulness and setting boundaries. Chronic stress can elevate cortisol, affect digestion, and weaken immunity—interfering with both health and test results.
These habits don’t guarantee I’ll never get sick, but they create a stronger foundation for early detection. When my body is functioning well, deviations from the norm stand out more clearly. That makes it easier for me—and my doctor—to catch problems before they escalate.
Breaking the “I Feel Fine” Myth: Why Waiting Is the Riskiest Move
One of the biggest barriers to early detection is the belief that “if I feel fine, I must be healthy.” I used to think that way. I avoided check-ups because I wasn’t sick. I assumed that no symptoms meant no problems. That mindset is common, but it’s also dangerous. Many serious conditions—high blood pressure, high cholesterol, type 2 diabetes, certain cancers—have no symptoms in their early stages. By the time symptoms appear, the disease may already be advanced.
Western medicine emphasizes preventive care precisely because the body often hides its struggles. Routine screenings are designed to uncover these hidden issues. Skipping them because you feel well is like refusing to service your car because it still runs. Eventually, small problems become big ones. The cost of waiting isn’t just financial—it’s measured in lost time, reduced treatment options, and lower quality of life.
Prevention isn’t reactive. It’s a long-term commitment to your well-being. It means showing up for appointments even when you’re busy, getting tests even when you’re not scared, and trusting science even when you feel fine. It’s not about living in fear of illness—it’s about living with confidence in your health.
My journey taught me that early detection isn’t passive. It requires action, consistency, and courage. It means paying attention, speaking up, and following through. But the reward is priceless: the peace of mind that comes from knowing you’re doing everything you can to protect your health.
Early detection isn’t about fear—it’s about freedom. By staying ahead with regular, science-based care, you gain control, clarity, and peace of mind. My journey taught me that the best health strategy isn’t waiting to fix problems, but preventing them from growing. This is the power of modern medicine, used wisely.