How I Tamed My Cholesterol—And Why It’s a Lifesaver
High cholesterol often flies under the radar—no pain, no warning. But inside, it’s silently setting the stage for heart issues. I learned this the hard way. After my doctor flagged my lipid levels, I dug into science-backed changes that actually work. This isn’t about quick fixes. It’s about real, sustainable shifts in how we eat, move, and live—steps that don’t just balance lipids, but protect your long-term health. What began as a routine checkup became a turning point, sparking a journey rooted in understanding, action, and resilience. The truth is, millions live with elevated cholesterol without knowing it, and by the time symptoms appear, damage may already be underway. The good news? With informed choices, this silent threat can be managed—effectively and permanently.
The Silent Threat: Understanding Cholesterol and Cardiovascular Risk
Cholesterol is a waxy, fat-like substance produced naturally by the liver and found in certain foods. Though often portrayed as harmful, it plays essential roles in building cell membranes, producing hormones, and aiding digestion. The real concern lies not in cholesterol itself, but in its balance. Blood lipid panels typically measure three key components: low-density lipoprotein (LDL), high-density lipoprotein (HDL), and triglycerides. Think of your bloodstream as a highway—LDL is like delivery trucks carrying cholesterol to tissues, but when there are too many, they can “overload” the road, depositing buildup along artery walls. This plaque narrows blood flow and increases the risk of clots, heart attack, and stroke.
HDL, on the other hand, acts like a cleanup crew, collecting excess cholesterol and returning it to the liver for removal. Higher HDL levels are generally protective. Triglycerides, another type of fat, store unused calories and provide energy between meals. When triglyceride levels rise—often due to excess sugar, alcohol, or calorie intake—they contribute to arterial stiffness and inflammation. The American Heart Association recommends keeping LDL below 100 mg/dL, HDL above 60 mg/dL, and triglycerides under 150 mg/dL for optimal heart health. However, these numbers can vary based on individual risk factors such as age, family history, and existing conditions like diabetes.
What makes high cholesterol so dangerous is its invisibility. Unlike conditions that cause pain or fatigue, dyslipidemia often shows no symptoms until complications arise. A person can feel perfectly fine while plaque silently accumulates over years. According to the World Health Organization, cardiovascular diseases are the leading cause of death globally, responsible for an estimated 17.9 million lives each year. A significant portion of these cases are linked to uncontrolled cholesterol levels. The risk isn’t limited to older adults—poor dietary habits and sedentary lifestyles are contributing to rising cholesterol levels even among younger populations. This underscores a crucial point: prevention must begin early, long before a diagnosis is made.
Understanding cholesterol isn’t about memorizing medical terms; it’s about recognizing that your daily choices influence this internal balance. Just as a car requires regular maintenance to run smoothly, your cardiovascular system depends on consistent care. The liver adjusts cholesterol production based on diet, but when saturated and trans fats dominate meals, it struggles to keep up. Over time, this imbalance leads to chronic inflammation and endothelial dysfunction—early signs of heart disease. The good news is that lipid levels are modifiable. Unlike genetics or age, diet, physical activity, and stress management are within reach. By treating cholesterol not as a distant medical concept but as a reflection of lifestyle, individuals gain the power to influence their long-term outcomes.
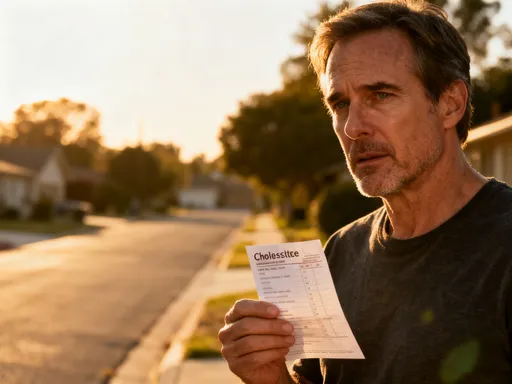
My Wake-Up Call: A Personal Turnaround Story
It started with a routine annual physical. I had no chest pain, no shortness of breath, and considered myself relatively healthy. I walked daily, cooked most meals at home, and avoided processed snacks. But when my doctor reviewed my blood work, she paused. “Your total cholesterol is 240, and your LDL is 160,” she said. “These are in the high-risk range.” I was stunned. At 48, with no family history of heart disease, I never imagined I’d be on that list. The numbers felt abstract, yet the concern in her voice was real. She explained that even without symptoms, these levels significantly increased my risk for cardiovascular events over the next decade.
In the days that followed, I cycled through confusion and worry. How could I feel fine while my body was silently at risk? I scoured the internet, only to be overwhelmed by conflicting advice—detox teas, miracle supplements, extreme diets. Some promised instant results, but none offered sustainable solutions. I realized that fear alone wouldn’t fix the problem; knowledge and action would. I scheduled a follow-up appointment and came prepared with questions. My doctor emphasized that while genetics play a role, lifestyle was the primary driver in most cases. She didn’t push medication immediately but encouraged a three-month trial of intensive lifestyle changes, with a repeat lipid panel to assess progress. This collaborative approach gave me hope—control was possible, but it required commitment.
What shifted my mindset was understanding that this wasn’t a failure, but an opportunity. My body was sending a message, and I could choose to listen. I began tracking my food, logging meals in a simple journal. I consulted a registered dietitian who helped me identify hidden sources of saturated fat—full-fat cheese, creamy dressings, even certain plant-based oils used in excess. I learned to read nutrition labels more critically, paying attention to trans fats and added sugars. At the same time, I increased my physical activity, starting with 20-minute walks and gradually building to 45 minutes most days. I also prioritized sleep, aiming for seven to eight hours nightly. These weren’t drastic changes, but consistent ones.
Three months later, I returned for another blood test. My total cholesterol had dropped to 205, and my LDL was now 128—still not ideal, but moving in the right direction. My HDL had increased slightly, and triglycerides had fallen by nearly 30 points. My doctor praised the progress and suggested continuing the current plan. This small victory reinforced a powerful truth: sustainable change is gradual, but it works. More importantly, I had taken responsibility for my health in a way I never had before. It wasn’t about perfection; it was about persistence. That experience transformed my relationship with wellness—from reactive to proactive, from anxious to empowered.
Diet Decoded: What Actually Moves the Needle on Lipids
Nutrition is one of the most powerful tools for managing cholesterol. While genetics influence baseline levels, diet can significantly shift the balance of LDL, HDL, and triglycerides. The key lies in understanding types of fat. Not all fats are created equal. Saturated fats, found in red meat, butter, full-fat dairy, and some tropical oils like coconut and palm oil, can raise LDL when consumed in excess. The American Heart Association recommends limiting saturated fat to no more than 5–6% of daily calories—for a 2,000-calorie diet, that’s about 13 grams per day. Trans fats, often listed as “partially hydrogenated oils” on labels, are even more harmful. They not only increase LDL but also lower HDL, creating a double risk. Though largely phased out of the U.S. food supply, they may still appear in some processed snacks, baked goods, and fried foods.
In contrast, unsaturated fats—both monounsaturated and polyunsaturated—are beneficial. These fats help reduce LDL and support HDL. Good sources include olive oil, avocados, nuts like almonds and walnuts, and seeds such as chia and flax. Omega-3 fatty acids, a type of polyunsaturated fat found in fatty fish like salmon, mackerel, and sardines, are particularly effective at lowering triglycerides and reducing inflammation. The American Heart Association recommends eating at least two servings of fatty fish per week. For those who don’t eat fish, plant-based sources like flaxseeds, walnuts, and algae-based supplements can provide some benefits, though they contain a different form of omega-3 (ALA) that the body converts less efficiently.
Fiber is another critical player. Soluble fiber, found in oats, barley, beans, lentils, apples, and citrus fruits, binds to cholesterol in the digestive system and helps remove it from the body. Studies show that consuming 5 to 10 grams of soluble fiber daily can lower LDL by about 5–10%. One easy way to increase intake is by starting the day with oatmeal topped with fruit. Plant sterols and stanols, naturally occurring compounds in plants, also block cholesterol absorption. They’re now added to some margarines, orange juices, and yogurt drinks. Consuming 2 grams per day of plant sterols can reduce LDL by up to 10%, according to clinical research.
Practical meal adjustments can make a meaningful difference without requiring a complete diet overhaul. For example, replacing butter with avocado on toast not only swaps saturated fat for heart-healthy monounsaturated fat but also adds fiber. Choosing grilled chicken instead of fried cuts down on trans and saturated fats. Swapping white rice for quinoa or brown rice increases fiber content. Even small substitutions, like using olive oil-based vinaigrette instead of creamy dressing, add up over time. The goal isn’t perfection but consistency. Occasional indulgences are fine—what matters is the overall pattern. Portion awareness also plays a role. Nuts, while healthy, are calorie-dense, so a small handful (about 1 ounce) is sufficient. Balancing nutrient-dense foods with mindful eating helps maintain progress without feeling deprived.
Move More, Stress Less: Lifestyle’s Hidden Power on Lipid Profiles
Physical activity is a cornerstone of lipid management. Exercise doesn’t just burn calories—it improves how the body processes fats and sugars. Regular movement increases HDL cholesterol, which helps clear excess cholesterol from the bloodstream. It also lowers triglycerides by improving insulin sensitivity and enhancing the body’s ability to use fat for energy. The good news is that you don’t need intense workouts to see benefits. Moderate activities like brisk walking, cycling, swimming, or dancing for at least 150 minutes per week can make a measurable difference. Strength training, performed two or more days a week, also supports metabolic health by increasing muscle mass, which in turn boosts resting calorie expenditure.
One of the most accessible forms of exercise is walking. It requires no special equipment, fits into most schedules, and can be done indoors or outdoors. Starting with 10 to 15 minutes a day and gradually increasing duration builds endurance without strain. Many find that walking after meals helps regulate blood sugar and supports digestion, indirectly benefiting lipid metabolism. Over time, increased activity leads to improved energy levels, better sleep, and enhanced mood—all of which support long-term adherence. The key is consistency, not intensity. Finding enjoyable activities increases the likelihood of sticking with them. Whether it’s gardening, dancing to favorite music, or joining a community fitness class, movement should feel sustainable, not punishing.
Equally important is managing stress and prioritizing sleep. Chronic stress triggers the release of cortisol and adrenaline, hormones that can raise blood pressure and increase blood sugar and fat levels. Over time, this contributes to weight gain, insulin resistance, and elevated triglycerides. Poor sleep—sleeping less than six hours or experiencing frequent disruptions—has similar effects. Research shows that adults who consistently get less than seven hours of quality sleep are more likely to have higher LDL and lower HDL levels. Sleep is when the body repairs tissues, regulates hormones, and balances metabolism. Disrupting this process undermines cardiovascular health.
Simple lifestyle strategies can help restore balance. Mindfulness practices such as deep breathing, meditation, or gentle yoga can reduce stress and improve emotional regulation. Even five to ten minutes a day can make a difference. Establishing a regular sleep routine—going to bed and waking up at the same time every day, avoiding screens before bedtime, and creating a calm sleeping environment—supports restful sleep. Limiting caffeine and alcohol, especially in the evening, also promotes better sleep quality. The compound effect of combining regular physical activity with improved stress management and sleep hygiene creates a powerful synergy. These elements don’t work in isolation; they reinforce one another, leading to broader improvements in overall health and well-being.
Beyond the Scale: Monitoring and Measuring Progress Right
Tracking progress is essential, but it requires the right approach. Lipid levels fluctuate naturally due to factors like recent meals, illness, stress, or even the time of day. This means a single blood test doesn’t tell the whole story. For most adults, the U.S. Preventive Services Task Force recommends screening every four to six years starting at age 20. However, those with risk factors—such as family history, high blood pressure, diabetes, or previous abnormal results—may need more frequent monitoring, typically every one to two years. After making lifestyle changes, a follow-up test in 8 to 12 weeks can provide early feedback, but long-term trends are more meaningful than short-term shifts.
It’s easy to become discouraged if numbers don’t drop quickly. However, lipid improvement is often gradual. A reduction of 20 to 30 points in total cholesterol over several months is a significant achievement. More importantly, small, sustained changes reduce cumulative risk over time. Beyond lab values, non-lab indicators offer valuable insights. Increased energy, better mood, improved sleep, and enhanced physical stamina are all signs of positive metabolic shifts. Some notice clothes fitting more loosely or feeling stronger during daily activities. These “wins” reinforce motivation and provide tangible evidence of progress, even before the next blood draw.
Keeping a wellness journal can help track both objective and subjective improvements. Logging meals, physical activity, sleep quality, and emotional state creates a holistic picture of health. Over time, patterns may emerge—such as better energy after certain foods or improved mood on days with more movement. This self-awareness supports informed decision-making and strengthens commitment. It’s also important to avoid comparing yourself to others. Individual responses to diet and exercise vary due to genetics, metabolism, and starting points. What matters is personal progress. Celebrating small milestones—like completing a month of daily walks or consistently choosing healthier fats—builds confidence and resilience.
Regular communication with a healthcare provider ensures that monitoring remains appropriate and safe. If lipid levels remain high despite lifestyle efforts, further evaluation may be needed. Some individuals have familial hypercholesterolemia, a genetic condition that causes very high LDL from birth and often requires medication. Others may have underlying conditions like hypothyroidism that affect lipid metabolism. A doctor can assess these possibilities and recommend next steps. The goal is not to obsess over numbers but to use them as tools for informed action—part of a broader strategy for lifelong heart health.
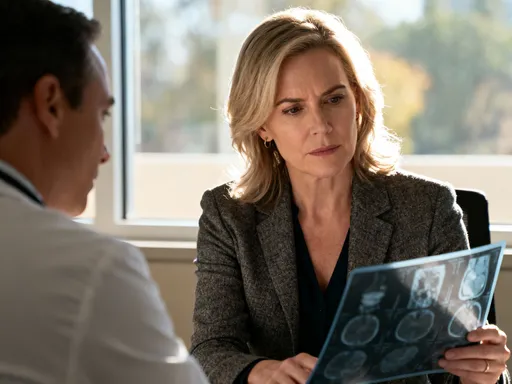
The Doctor’s Role: Why Professional Guidance Is Non-Negotiable
While lifestyle changes are powerful, they are not always sufficient on their own. A healthcare provider plays a critical role in evaluating individual risk, interpreting test results, and determining the best course of action. Cholesterol management is not one-size-fits-all. Age, gender, family history, blood pressure, and the presence of conditions like diabetes all influence treatment decisions. Doctors use risk assessment tools, such as the ASCVD (Atherosclerotic Cardiovascular Disease) risk estimator, to calculate a person’s 10-year risk of heart attack or stroke. This helps determine whether lifestyle changes alone are enough or if medication—such as statins—is recommended.
Statins are among the most studied and effective medications for lowering LDL cholesterol. They work by inhibiting an enzyme in the liver that produces cholesterol, thereby reducing circulating levels. Numerous clinical trials have shown that statins significantly reduce the risk of heart attack and stroke, even in people without prior cardiovascular events. Despite their proven benefits, some individuals hesitate due to concerns about side effects. Muscle pain is the most commonly reported issue, but serious side effects are rare. For most, the benefits far outweigh the risks, especially when monitored by a physician. Other medications, such as ezetimibe or PCSK9 inhibitors, may be used in combination or for those who cannot tolerate statins.
It’s important to view medication not as a failure of lifestyle efforts but as a complementary tool. Just as insulin helps manage diabetes or inhalers support asthma control, cholesterol-lowering drugs are part of a comprehensive approach. The decision to start medication should be made collaboratively, with open discussion about goals, concerns, and expectations. Doctors can also rule out secondary causes of high cholesterol, such as kidney disease, liver dysfunction, or certain medications like steroids or beta-blockers. They may recommend additional tests, such as a coronary calcium scan, to assess existing plaque buildup.
No supplement, diet trend, or fitness app can replace a clinical evaluation. While some natural products like red yeast rice contain compounds similar to statins, they are not regulated like prescription drugs and may vary in potency or interact with other medications. Similarly, over-the-counter “cholesterol support” supplements often lack strong evidence. The safest and most effective path is through professional care. Regular checkups, honest conversations, and shared decision-making build a foundation of trust and accountability. Viewing your doctor as a partner—not an authority figure to fear—empowers you to take charge of your health with confidence.
Building a Heart-Healthy Life: Small Steps, Big Impact
Managing cholesterol is not a short-term project; it’s a lifelong commitment to heart health. The choices that lower lipids—eating more whole foods, moving regularly, sleeping well, and managing stress—also reduce the risk of other chronic conditions like type 2 diabetes, obesity, and certain cancers. This creates a ripple effect: improving one aspect of health often enhances many others. The journey doesn’t require drastic overhauls. Lasting change comes from small, sustainable steps that become habits over time. The goal is progress, not perfection.
A simple starter plan can make the path forward feel manageable. Begin with one food swap—replace butter with olive oil, choose whole grains over refined ones, or add a serving of vegetables to dinner. Add one daily walk, even if it’s just 10 minutes. Incorporate one stress-reset practice, such as deep breathing, journaling, or listening to calming music. These actions may seem minor, but their cumulative impact is profound. Over weeks and months, they reshape routines, strengthen resilience, and build confidence. As new habits take root, additional changes become easier to adopt.
Creating a supportive environment also increases success. Stock the kitchen with healthy staples—oats, beans, frozen vegetables, nuts, and heart-healthy oils. Prepare simple meals in advance to reduce reliance on convenience foods. Involve family members by cooking together or taking evening walks as a group. Social support enhances motivation and makes healthy living more enjoyable. Sharing experiences, challenges, and victories fosters connection and accountability.
Finally, remember that every positive choice counts. You don’t have to do everything at once. Each meal, each step, each mindful breath is a vote for your future health. Cholesterol may be silent, but your actions speak loudly. By making informed, consistent choices, you take control of your well-being and protect the life you cherish. Heart health isn’t just about numbers on a lab report—it’s about vitality, energy, and the freedom to live fully. And that’s a promise worth keeping.