How I Rebuilt My Strength: A Real Talk on Daily Rehab Habits
Recovery isn’t just about healing—it’s about building a life that supports your body every single day. After my own rehab journey, I learned that small, consistent habits make the biggest difference. This isn’t a quick fix, but a real, science-backed approach to daily health. If you're rebuilding strength or supporting recovery, this is for you—no hype, just honest insights from experience and professional understanding. It’s time to shift how we think about rehabilitation: not as a temporary phase, but as a permanent foundation for a stronger, more resilient life.
The Hidden Struggle Behind Recovery
Many people believe that rehabilitation ends when formal therapy sessions stop. They expect to walk out of physical therapy fully restored, ready to return to life as it was before injury or surgery. But the truth is far more complex. The real challenge begins after the last appointment—when the structured guidance fades and daily life takes over. Without continued support, individuals often face unexpected fatigue, lingering stiffness, and a deep-seated fear of re-injury. These emotional and physical hurdles can be overwhelming, especially when no one prepares you for them.
One of the most common misconceptions about recovery is that it follows a linear path. In reality, healing is rarely a straight line. It comes with setbacks, plateaus, and moments of doubt. A person might feel strong one day and struggle the next, not because they’ve done something wrong, but because the body heals in waves. Traditional rehab programs, while valuable, often conclude too early—before patients have developed the confidence or tools to manage these fluctuations on their own. This gap leaves many feeling abandoned, unsure of how to proceed.
Another overlooked aspect is motivation. After weeks or months of effort, it’s natural to want to stop once progress slows. But stopping at the first sign of stability can undermine long-term gains. The body adapts to what it’s asked to do. If movement decreases too soon, muscles weaken, joints stiffen, and coordination declines. That’s why the transition from passive treatment to active self-care is so critical. Rehabilitation must evolve from something done *to* you into something you do *for* yourself, every day.
The shift from patient to empowered individual requires a mindset change. Instead of waiting for permission to move, people need to learn how to listen to their bodies, recognize warning signs, and adjust accordingly. This doesn’t mean pushing through pain or ignoring limits—it means developing awareness and making informed choices. When recovery becomes part of daily living, rather than a separate task, the chances of lasting improvement increase dramatically.
Why Daily Habits Define Long-Term Success
Long-term recovery isn’t built in the clinic—it’s built at home, in the kitchen, during walks, and in the way you sit, stand, and sleep. The key to sustainable strength lies not in intense weekly workouts, but in the small, repeated actions that shape your day. Science supports this: neuroplasticity—the brain’s ability to reorganize and form new neural connections—thrives on consistency. Similarly, muscle memory is reinforced through repetition, not isolated efforts. This means that daily movement, even in modest amounts, has a compounding effect over time.
Consider two individuals recovering from knee surgery. One attends therapy twice a week but remains largely inactive otherwise. The other integrates short walks, gentle stretches, and posture checks throughout each day. Over six weeks, the second person may not seem dramatically stronger at first, but by three months, they are more likely to walk without hesitation, climb stairs with ease, and report less discomfort. Why? Because their nervous system and musculature have been consistently engaged, reinforcing proper movement patterns.
Research published in journals like the *Archives of Physical Medicine and Rehabilitation* shows that patients who maintain structured daily activity after formal therapy are significantly more likely to retain functional gains. These habits don’t need to be complex or time-consuming. What matters is regularity. A five-minute stretch in the morning, a mindful walk after lunch, or deliberate breathing before bed—all contribute to a system that supports healing.
Contrast this with sporadic exercise. Going all-out on weekends while being sedentary the rest of the week creates imbalance. It increases the risk of strain and sends mixed signals to the body. The musculoskeletal system responds best to predictable, moderate input. Daily habits provide that stability. They train the body to expect movement, reduce inflammation through circulation, and maintain joint lubrication. Over time, this routine becomes invisible—a natural part of life, like brushing your teeth or drinking water.
Movement as Medicine: Rethinking Physical Activity
Physical activity during recovery shouldn’t be limited to prescribed exercises. Every movement counts. Functional movement—activities that mimic real-life actions like reaching, bending, lifting, and balancing—plays a vital role in rebuilding strength and confidence. These aren’t just tasks; they are opportunities to reinforce healing. When done with awareness, everyday motions become therapeutic. For example, standing up from a chair can be an exercise in core engagement and leg strength. Carrying groceries can improve grip and shoulder stability—if done with proper form.
The concept of “movement snacking” has gained attention in rehabilitation science. Just as small, nutritious snacks keep energy steady throughout the day, short bursts of intentional movement can keep the body active and responsive. A two-minute walk every hour, a set of seated marches, or wall push-ups while waiting for the kettle to boil—these micro-movements add up. They prevent stiffness, stimulate blood flow, and remind the nervous system how to coordinate muscle groups. Unlike long, exhausting sessions, movement snacks are sustainable and adaptable, even on low-energy days.
Posture also matters during daily tasks. Many people unknowingly strain their bodies while doing household chores. Leaning over the sink to wash dishes, twisting to unload the dishwasher, or bending at the waist to pick up laundry can place unnecessary stress on the spine and joints. Simple adjustments—using a small stool to elevate one foot, keeping the back straight when lifting, or organizing frequently used items at waist level—can make a significant difference. These changes reduce wear and tear, protect healing tissues, and promote long-term joint health.
Pacing is another essential strategy. Pushing too hard on a good day often leads to increased pain or fatigue the next. This cycle discourages consistency. Instead, pacing involves breaking tasks into manageable segments with rest in between. For instance, folding laundry in two 10-minute sessions instead of one 20-minute stretch allows the body to recover between efforts. This approach prevents flare-ups and supports steady progress. When movement is balanced with rest, the body learns to trust the process, reducing fear and increasing participation.
The Mind-Body Connection in Recovery
Healing is not just physical—it’s deeply influenced by mental and emotional states. Chronic stress, poor sleep, and mental fatigue can slow tissue repair, increase pain sensitivity, and weaken immune function. The nervous system, when under constant stress, releases cortisol and other hormones that promote inflammation. This biological response, meant for short-term survival, becomes harmful when sustained over time. For someone in recovery, this means that even with perfect exercises and nutrition, unresolved stress can hinder progress.
Mindfulness and breathwork offer powerful, accessible tools to counter this. Diaphragmatic breathing, for example, activates the parasympathetic nervous system—the “rest and digest” mode. Just a few minutes of slow, deep breaths can lower heart rate, reduce muscle tension, and improve oxygen delivery to tissues. Practicing this before bedtime or during moments of discomfort helps the body shift from a state of alertness to one of restoration. It’s not about eliminating stress entirely, but about building resilience to it.
Body scans are another effective technique. This practice involves mentally checking in with different parts of the body, noticing sensations without judgment. It enhances body awareness, which is often diminished after injury. When people reconnect with their physical selves, they become better at detecting early signs of strain or imbalance. A body scan can be done lying down before sleep or sitting quietly with eyes closed. Starting at the toes and moving upward, the focus is on observation, not correction. Over time, this builds a kinder, more attentive relationship with the body.
Sleep quality is equally important. During deep sleep, the body repairs tissues, consolidates motor learning, and regulates hormones. Poor sleep disrupts these processes, making recovery slower and more painful. Creating a calming bedtime routine—dimming lights, avoiding screens, practicing gentle stretching or breathing—signals the body that it’s time to rest. Consistent sleep and wake times, even on weekends, support circadian rhythm and improve overall healing capacity. When mental and physical routines align, recovery becomes more efficient and sustainable.
Designing Your Personalized Daily Routine
There is no one-size-fits-all rehab plan. Each person’s journey is shaped by their injury, lifestyle, energy levels, and goals. That’s why creating a personalized daily routine is essential. The foundation of such a routine includes timing, duration, and progression. For example, someone recovering from shoulder surgery might start with five minutes of gentle range-of-motion exercises in the morning and evening. As strength improves, they can gradually increase duration or add resistance—always within safe limits.
Timing matters. Some people feel stiff in the morning and benefit from light movement upon waking. Others find midday activity helps break up sedentary time. The key is to align movement with natural energy patterns. A routine shouldn’t feel like a burden. If morning stretches are overwhelming, doing them after a warm shower—when muscles are more pliable—may work better. Flexibility in scheduling increases adherence.
Progression should be gradual. The principle of “just enough” applies: challenge the body slightly beyond its comfort zone without triggering pain or fatigue. This might mean adding one more repetition, holding a stretch a few seconds longer, or walking a little farther. Tracking progress doesn’t have to involve numbers. Paying attention to how clothes fit, how easily you climb stairs, or how rested you feel in the morning provides meaningful feedback. These subtle indicators often reflect real improvement better than a stopwatch or tape measure.
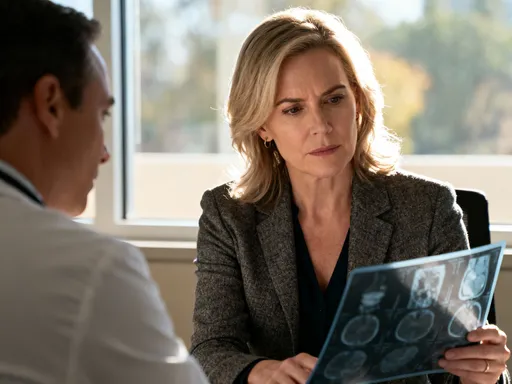
Professional guidance remains crucial. Working with a physical therapist or certified trainer ensures that exercises are appropriate and performed correctly. They can help modify routines as needed and identify potential risks before they become problems. Regular check-ins, even brief ones, provide accountability and reassurance. A personalized plan isn’t static—it evolves as you do, adapting to changes in health, schedule, or environment.
Nutrition and Recovery: Fueling the Healing Process
Food is medicine, especially during recovery. The body needs specific nutrients to repair tissues, reduce inflammation, and maintain energy. Protein is essential—it provides the building blocks for muscle and connective tissue. Good sources include lean meats, fish, eggs, dairy, legumes, and plant-based proteins like tofu and lentils. Including a source of protein with every meal helps support continuous repair throughout the day.
Hydration is equally vital. Water makes up a large portion of muscles, joints, and connective tissues. Even mild dehydration can lead to stiffness, reduced circulation, and fatigue. Drinking water consistently—not just when thirsty—keeps tissues supple and supports metabolic function. Herbal teas, broths, and water-rich fruits and vegetables also contribute to fluid intake.
Anti-inflammatory foods play a supportive role. Chronic inflammation can delay healing and increase pain. Foods rich in omega-3 fatty acids—such as salmon, walnuts, and flaxseeds—help balance the body’s inflammatory response. Colorful fruits and vegetables—berries, spinach, carrots, and sweet potatoes—are packed with antioxidants that protect cells and support immune function. Whole grains, nuts, and seeds provide sustained energy and essential minerals like magnesium, which aids muscle relaxation.
Meal timing can enhance recovery. Eating smaller, balanced meals throughout the day helps maintain steady blood sugar and energy levels. A light snack containing protein and healthy fats—like Greek yogurt with berries or apple slices with almond butter—about 30 minutes before or after activity can support muscle recovery and prevent fatigue. Avoiding large, heavy meals prevents sluggishness and supports digestion. Nutrition isn’t a separate track from rehab—it’s woven into the same fabric. When food choices align with healing goals, the body has the resources it needs to rebuild strength from the inside out.
Staying on Track: Overcoming Setbacks and Staying Motivated
Setbacks are a normal part of recovery. A sudden increase in pain, a day when movement feels harder, or a missed routine doesn’t mean failure—it means you’re human. The key is not to avoid setbacks, but to respond to them with compassion and wisdom. Instead of reacting with frustration, ask: What changed? Did I do too much yesterday? Am I not sleeping well? Is stress higher than usual? These reflections help identify triggers and make adjustments without self-blame.
When progress stalls, it’s important to revisit your routine. Maybe it’s time to reduce intensity, change the type of activity, or add more rest. Sometimes, a short break is needed to allow the body to catch up. Other times, seeking professional advice can uncover underlying issues. A physical therapist might suggest a new exercise, a doctor might check for nutritional deficiencies, or a counselor might help manage stress. Asking for help is not weakness—it’s a sign of commitment to long-term health.
Motivation ebbs and flows. On hard days, focusing on small victories helps maintain momentum. Did you do your breathing exercises? Did you drink enough water? Did you rest when you needed to? These choices matter. Setting realistic, process-oriented goals—like “move for 10 minutes every day” instead of “walk three miles”—keeps expectations achievable. Celebrating consistency, not perfection, builds confidence over time.
Ultimately, rehabilitation is not a race. It’s a lifelong commitment to feeling stronger, more capable, and more in tune with your body. The habits you build today lay the foundation for tomorrow’s resilience. They are not just about recovering from an injury—they’re about creating a life where strength, balance, and well-being are the norm. Every small choice adds up. And over time, those choices transform not just your body, but your entire relationship with health.